Impingement Syndrome
What is it?
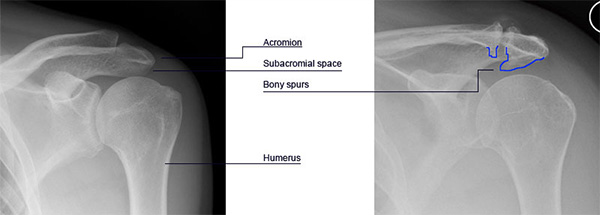
The shoulder is raised or lowered by a group of four muscles (supraspinatus, infraspinatus, subscapularis and teres minor), which are called the ‘rotator cuff muscles’. These muscles lie in a space between the top of the arm bone (humerus) and the shoulder blade (the acromion). This space is called the ‘subacromial space’ and a fluid-filled sac (the subacromial bursa) fills it. This fluid sac allows for smooth gliding of the rotator cuff muscles under the spine of the shoulder blade, when the shoulder moves. In certain conditions the rotator cuff or the bursa can get pinched between the humeral head and the acromion. This causes inflammation and fluid formation within the space resulting in a set of symptoms, which are described as ‘subacromial impingement syndrome’.
Is it called by any other name?
Shoulder Bursitis, Shoulder Tendonitis, Trapped Tendons, Shoulder strain.
What is the cause?
Normal wear and tear of the muscles, injury to the rotator cuff, repeated overhead movements, sudden (unused & improper) lifting or poor posture can cause inflammation of the rotator cuff causing impingement. Similarly with age, bone spurs may develop under the end of the collarbone or the spine of the shoulder blade (picture below) resulting in reduced subacromial space. Some people have a more curved acromion, which is susceptible to such impingement. In sportspersons who do a lot of overhead activity the undersurface of the rotator cuff may get pinched in certain positions of throwing causing pain. This is called internal impingement and such a condition differs from subacromial impingement.
What are the symptoms and how is the condition diagnosed?
The main complaint is of pain, a pinching sensation and stiffness when the patient raises the arm. The pain is usually experienced in the upper arm and generally worsens at night. The symptoms make it difficult to do overhead work (such as comb your hair), and also restricts movements (like putting your hand behind your back) and sleeping on the affected side.
Will further tests or investigations be needed?
Further investigations (x-rays, ultrasound or an MRI scan) may be recommended. These investigations will help to determine the shape of the acromion, presence of any bony spurs or arthritis and the integrity of the rotator cuff muscles.
What is the treatment?
- In the initial stages painkillers and anti-inflammatory medication will be useful. Activities that aggravate the symptoms should be avoided or modified.
- Physiotherapy is usually the first line of treatment. You will be taught specific exercises designed to reduce irritation of the rotator cuff, improve flexibility of the muscles and provide balanced shoulder strength.
- An injection of steroid and local anaesthetic is considered either before or after physiotherapy depending on the symptoms. The steroid injection reduces inflammation and controls the pain. Improvement is variable and can be temporary. It is important that you are assessed a few weeks later and the response to the injection analysed.
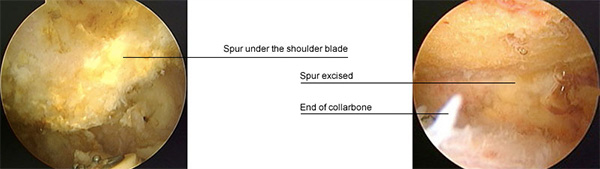
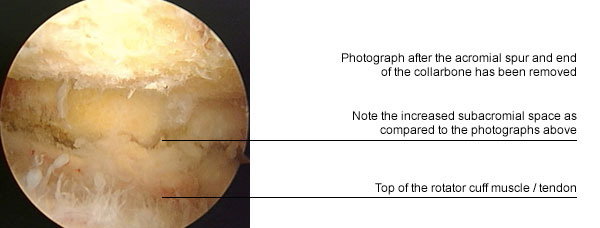
- If the symptoms have not responded to the above treatment then surgery may be required. The standard operation advised nowadays is an arthroscopic ‘subacromial decompression’ (keyhole surgery). The aim of the operation is to increase the size of the subacromial space and reduce the pressure on the rotator cuff. About 2-3 small stab incisions are made around the shoulder through which a telescope (arthroscope) is passed. The surgery is seen on a television monitor. It involves partial removal of the subacromial bursa, cutting one of the ligaments that is reducing the space, and shaving away the bony spurs. This will release the pressure on the trapped tendon or bursa so the cuff can move smoothly. The advantage of keyhole surgery is that tiny incisions are needed; the rehabilitation is quicker and any other pathology (rotator cuff tear, biceps) can also be identified and treated. At surgery you will be given a regional anaesthetic block. This will cause numbness for approximately 24 hours. The aim of the block is to give pain relief following surgery and make the postoperative period comfortable. Following surgery you will have a large compression dressing and a shoulder sling for comfort. You can discard the sling after 2-3 days.
What happens if it is not treated?
It is likely that the symptoms will linger indefinitely. As the space narrows and the tendons continue to get pinched the tendons may tear. This may lead to loss of ability to actively lift the arm.
What is the success of surgical treatment?
The operation has a good success rate. Most patients see a dramatic and rapid improvement of their symptoms within a few weeks of surgery. Generally within three weeks of surgery, movement above the level of the shoulder becomes more comfortable. Within about 3 months, your symptoms should be about 80% improved and you should continue to improve for up to one year following the procedure.
What are the complications of surgical treatment?
- Infection of the wound is possible. This is very rare in arthroscopic shoulder surgery and if it does happen it can be successfully treated with antibiotics.
- Shoulder stiffness is possible and hence it is important to follow the physiotherapy rehabilitation after surgery.
- Any surgical intervention has a risk of developing complications that are unpredictable. These complications may have the potential to leave the patient worse than before surgery.
Is there anything I can do to improve outcome?
In the initial days after surgery the wound should be kept dry. Following surgery it is important to maintain correct posture and be compliant with postoperative exercises. I would advise against wearing rings on the operated side for 4-6 weeks following surgery.
When can I do various activities?
- Return to work depends on many factors including the nature of the job and hand dominance. Generally patients can return to a desk job within 7-10 days of surgery. If you are involved in manual work, then a longer period can be expected.
- You should avoid sustained repetitive overhead work for at least 3 months following surgery. You could return to swimming (breast stroke) as soon as comfortable but you should wait for at least 3 months before resuming front crawl.
- Driving should be possible within a week of the operation.


 MENU
MENU





